Not Seeing ME/CFS: A Failure of the American Medical System
By James Holcomb / Fall 2020
Although Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) has been viewed as a mental illness for decades, there has been evidence since at least the 1990s that ME/CFS is a physiological disease. Only now are people, government administrators, and healthcare workers beginning to see it as the complex, disabling, neuroimmune disease it is. ME/CFS impacts about up to 3.7 million in the U.S. (Valdez et al.). Of those, about twenty percent are classified as severe which means that they are mostly bedbound, and functionally limited. This staggeringly large number of people affected by ME/CFS in the U.S. alone can be analyzed better when compared to another highly prevalent disease, such as HIV/AIDS. Approximately 1.2 million people in the U.S. are living with HIV today (HIV.gov), which is about one-third of the ME/CFS individuals. This comparison becomes even more important when viewing the multiple orders of magnitude difference in research funding for ME/CFS compared to AIDS.
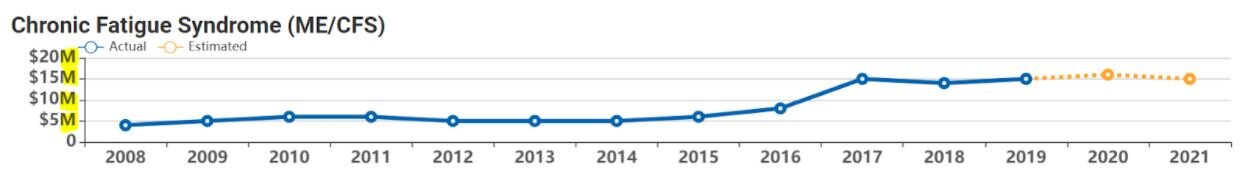
(NIH Categorical Spending Report, 2020) NOTE: Since about three times as many people have ME/CFS as have HIV/AIDS - this gap is about three times as big when research funding dollars per patient is considered. In 2020, HIV/AIDS research funding would be calculated as $2,531 per patient while ME/CFS research funding would be $4.32 per patient. Additionally, HIV/AIDS patients are eligible for a vast array of federal, state, and sometimes local funding for housing, food, prescriptions, insurance, and medical services, while none of this funding is available to people with ME/CFS (Resources for People living with AIDS).
Initially HIV/AIDS was frequently a death sentence but now there are treatments and many people live and function normally with it. A leading ME/CFS and HIV/Aids researcher and physician said “But I hope you are not saying that C.F.S. patients are not as ill as H.I.V. patients. My H.I.V. patients for the most part are hale and hearty thanks to three decades of intense and excellent research and billions of dollars invested. Many of my C.F.S. patients, on the other hand, are terribly ill and unable to work or participate in the care of their families.
I split my clinical time between the two illnesses, and I can tell you if I had to choose between the two illnesses I would rather have H.I.V. But C.F.S., which impacts a million people in the United States alone, has had a small fraction of the research dollars directed towards it.” (Klimas).
Thus ME/CFS impacts a significant sub-population of people and is both more disabling than similar diseases such as HIV/AIDS, and far less funded (around 0.1-0.05% of the funding). This is becoming even more topical recently as COVID ‘long-haulers’, as they are being termed, are now being diagnosed with ME/CFS after suffering from the same symptom complex for six months, which is increasing the general prevalence of it within our population.
One of the larger reasons ME/CFS is not as widely recognized and researched today despite the prevalence and severity the disease holds is that it had an awful debut in public media. The disease has a very diverse range of symptoms and many of them are not visibly expressed. Just like what originally happened regarding depression and many things similar to it, such as multiple sclerosis, when it was first known as “hysterical paralysis” brought on by “oedipal fixations,” until later investigations found it to be an immunological disease. (Siegel et al.) ME/CFS has been categorized as a mental illness that can be “treated” by exercise and positive thoughts. This life-altering disease was laughed at and made fun of instead of being seriously researched.
In the late eighties, newspaper and magazine articles began appearing about this disease. Most included pictures of tired looking white women and quickly the disease became known as the “rich white woman's disease”. (Jenkins) Other names included “Raggedy Ann Syndrome'', and “Yuppie Flu”. “highly reputable outlets like Newsweek and The Washington Post wrote pieces with stigmatizing headlines such as ‘Yuppie Flu – The Fatigue That Never Ends.’ These headlines were then recycled by several other media outlets, thus influencing public opinion of the illness, perpetuating the notion that people with CFS are weak-willed or suffering from psychosomatic illness.” (Siegel et al). Statistics have since shown that there was no racial or wealth discrimiation between the disease, but that lower class citizens were noticed to have a harder time getting diagnosed. However, these statistics became largely drowned out through large media to most people, and even more problematically, to the clinical specialists in charge of diverse areas. The stigma that this disease was exclusively for white women only made getting a real diagnosis for this disease even harder for minorities. (Jenkins) Men also suffer because of this inaccurate depiction, even though 35-40% of diagnosed patients are male. (Valdez et al.)
Corporations have benefited from ME/CFS’ diminishment. As explained in the movie “Merchants of Doubt”, large corporations are willing to spend great sums of money to sway public opinion in their favor. In “Merchants of Doubt” we saw examples of how neoliberalism has shifted power to large corporations and away from health and safety of the individual. One such example of this from the Tobacco industry and Flame Retardant industry’s abuses of power, and this can be analyzed in regards to ME/CFS. Medical healthcare groups and insurance companies have used the fact that ME/CFS does not have any official tests or treatments to deny services to sick people. Insurance companies have not covered treatments, therapies, or tests because there are no official strategies to positively test for ME/CFS even though the guiding statement has been to treat symptoms. This means anyone trying to work with an ME/CFS specialist will have to pay out of pocket as most potential treatments or therapies are categorized as ‘experimental’, further discriminating against lower-income minorities.
Healthcare groups have not updated their diagnostic criteria because if they do, they will have patients who are diagnosed with ME/CFS and then will require treatments. My mother’s physician at Kaiser got in trouble for trying to help her find treatment even though her diagnosis was prior to her becoming a KP patient. He was told that Kaiser didn’t diagnose patients with ME/CFS because then they would have to have a treatment plan. Kaiser in Northern California had a doctor designated to work on ME/CFS but he retired. According to members of the facebook group Kaiser ME Neglect Movement who have been trying to get KP to treat ME/CFS patients since May 2018 with very little success, the doctors listed in the Southern California directory for patients won’t treat patients with anything other than discredited Cognitive Behavioral Therapy (CBT) or Graded Exercise Therapy (GET). CBT and GET have been found ineffective at best for ME/CFS patients (Smith et al) and at worst GET can actually be dangerous for them (Doucleff).
An additional reason corporations are disincentivized from recognizing ME/CFS is most doctors have very little knowledge of ME/CFS and training them would be costly. A minority of medical schools (Peterson et al.) or medical textbooks (Jason et al.) cover the disease. Our healthcare industry has a very apparent hole when it comes to ME/CFS, and instead of trying to fill these gaps in knowledge or help this forgotten minority, the public turns them into enemies instead. It is very common for people suffering from ME/CFS to attempt to inform themselves of all available studies and knowledge about their disease and then be told by their respective doctors that their symptoms are all in their head. This obviously leads to a point of contention between doctor and patient, and has resulted in a labeling of ME/CFS patients as ‘militant’. “Scrutinizing this charge, we find no compelling evidence that the vast majority of patients with ME/CFS, or the POs representing them, have adopted any such militant political policies or behaviours… We find that widespread negative stereotyping of patients and the marginalization and exclusion of patient voices by medical authorities provides a better explanation for expressions of frustration among patients with ME/CFS” (Åsbring et al.)
Lastly, if ME/CFS does get recognized more widely as a disability, corporations will be required to not discriminate against ME/CFS patients which would possibly retool their HR Policies. “Another major misconception Walters has had to contend with is the cost of hiring those with disabilities. Many employers assume their healthcare expenses and insurance premiums will skyrocket, despite the fact that Medicare, Work Opportunity Tax Credits, the Ticket to Work program, and other government initiatives bear most of the financial burden.” (Linzon)
Minorities, underserved, and low income patients have been shown to be impacted by ME/CFS worse than most. They are less likely to be diagnosed, or receive treatments or accommodations if they are diagnosed but additionally, environmental factors can also make them more likely to be triggered or have worse ME/CFS symptoms. “‘Despite the heterogeneity of CFS, [and] the diversity of factors that lead to this condition, our findings show that the cellular metabolic response is the same in patients,’ said Naviaux. ‘And interestingly, it’s chemically similar to the Dauer state you see in some organisms, which kicks in when environmental stresses trigger a slow-down in metabolism to permit survival under conditions that might otherwise cause cell death. In CFS, this slow-down comes at the cost of long-term pain and disability.’” (Hrala) Pollution, allergens, temperature and other harmful environmental factors all can act as triggers for ME/CFS or may worsen existing illness. This makes victims of environmental racism more likely to suffer from ME/CFS or get sicker from it which means low-income communities are disproportionately affected. "Many of these problems face low-income communities as a whole, but race is often a more reliable indicator of proximity to pollution." (Beech)
While I’ve been talking a lot about how ME/CFS can be more dangerous and active among minorities, it is important to realize that patients suffering from ME/CFS are a silent minority themselves. The disease can commonly be severe enough for the victims to be fully bedridden which, combined with the lack of obvious symptoms led to the labeling of ME/CFS as an “invisible illness”. This new minority displays most of the common silencing tactics seen in our classes material for racial and religious minorities. Between the smear campaigns that trivialize this disease as a minor mental illness, now-discredited research, and the inability for the disabled individuals to participate in rallies, this minority goes largely unheard.
At this point you may be starting to adopt a popular opinion that this disease seems incredibly unfair, and that receiving a diagnosis of ME/CFS can to some feel worse than a death sentence. It is incredibly easy to become depressed after being diagnosed with this chronic illness. However since the history of ME/CFS is filled with it being wrongly considered a mental illness, patients often have to hide the depressing nature of the disease out of fear of having their symptoms being considered “all in their head”. The stigmas we have in society are making this disease harder to be treated, as it has been stereotyped even by some doctors as being inconsequential. As American’s we have a sad history and unfortunate talent at taking things we do not fully understand and describing them as lesser. A large subset of American people are known to have discriminatory actions and thoughts towards minorities, which is demonstrated by our history of continuous poor treatment and stereotyping of immigrants and people suffering from mental illnesses.
The facts need to be spread that this disease is real and the people being affected by it need our help and support. The notion that ME/CFS is a disease somehow exclusive to white people is actually just causing harm to minorities who cannot receive the diagnosis they are looking for and this needs to change. A large number of Americans are having their lives halted by a disease that is still considered fantasy by many doctors. The people that desperately need to have their voices heard are stuck in bed, some having to use feeding tubes, unable to speak their part. To help save these people we have to speak for them and let their voices be heard. We as fellow humans have to use the peaceful measures we have been slowly learning and perfecting to get the message out, that ME/CFS is a real disease and REQUIRES us to treat it, and those suffering from it, with respect as we attempt to help them. Since 2015, MEAction has annually sponsored a “Millions Missing” action in May during which shoes are displayed worldwide to signify the ME/CFS people missing from leading regular lives. This action is poignant because most patients are unable to advocate or attend but their shoes stand in for their voices (News MEAction).
The risk of some diseases like AIDS, or heart disease can be reduced if you diet correctly, make different decisions regarding sexual health, or other sorts of lifestyle choices. There is no lifestyle choice that has been found to reduce the risk of ME/CFS, which appears to be triggered by viruses (which currently seems to include COVID-19), environmental, physical or other stressors. It is important that we learn about this disease, as while it may have genetic links, it could happen to you or someone you care about, without any warning. This disease has a significant financial impact on our country and world as the people suffering from it generally cannot continue working. People diagnosed with moderate to severe ME/CFS usually cannot keep up full-time schooling or careers and often need to have care-givers. Students who are well enough to attend school have difficulty getting necessary accommodations because of the difficulty in getting diagnosed, challenges getting a doctor who will work with a school, and misperceptions by school administrations. While those with more severe cases of ME/CFS are often bedbound and relegated to minimal sensory environments with little contact, are sometimes on feeding tubes and usually require home nursing assistance.
One of the hardest things to accept when you get sick with ME/CFS is that your life has unalterably changed. You are no longer able to reach the goals you have set or manage “normal” everyday life, even as a mildly ill ME/CFS person. This reminded me of something I read from Professor Twohig: “For me, the thought grew out of social standards that I was trained to accept as a measure of my success.”. Between the pain and symptoms, and the revised self-image, people with ME/CFS are up to six times more likely to commit suicide than the general population. (Roberts)
The Quality of Life index
The Quality of Life index graph shown ranks ME/CFS lowest compared to other diseases and conditions. (Hvidberg et al.) Researching and coming up with treatments to ME/CFS therefore could have a very high return on investment, as treating it can potentially free up a lot more able-bodied individuals to be healthy and capable of contributing to society. “The direct and indirect economic costs of ME/CFS to society have been estimated at $17 to $24 billion annually (6), including $9.1 billion attributed to lost household and labor force productivity” (Valdez et al.)
On top of the personal and economic motivations, people should be more concerned about ME/CFS simply because helping these people who cannot help themselves should be an inherent part of our society. In order to progress towards a more idyllic and morally upright country, we must take actions that uphold the beliefs our desired nation should stand for. And what more worthy fight is there than to make the world a better place while helping to alleviate the suffering of people who are unable to fight for themselves?
Works Cited
Beech, Peter. “What Is Environmental Racism and How Can We Fight It?” World Economic Forum, The International Organization for Public-Private Cooperation, 31 July 2020.
Doucleff, Michaeleen. “For People With Chronic Fatigue Syndrome, More Exercise Isn't Better.” NPR, NPR, 2 Oct. 2017.
HIV.gov “U.S. Statistics.” HIV.gov, 5 Nov. 2020.
Hrala, Josh. “Chronic Fatigue Syndrome Appears to Leave a 'Chemical Signature' in The Blood.” ScienceAlert, Science Alert, 31 Aug. 2016.
Hvidberg, Michael Falk, et al. “The Health-Related Quality of Life for Patients with Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS).” PLOS ONE, Public Library of Science, 5 July 2016.
Jason, Leonard A, et al. “Frequency and Content Analysis of Chronic Fatigue Syndrome in Medical Text Books.” Australian Journal of Primary Health, U.S. National Library of Medicine, 2010.
Jenkins, Wilhelmina. “Race, Ethnicity and M.E.: Why We Need to Build a More Inclusive Movement and Why It Matters.” #MEAction Network, MEAction, 21 July 2020.
Kenner, Robert, director. Merchants of Doubt: L'industria Del Dubbio. Merchants of Doubt, Sony Pictures Home Entertainment, 2015.
Klimas, Nancy. “Readers Ask: A Virus Linked to Chronic Fatigue Syndrome.” The New York Times, The New York Times, 15 Oct. 2009.
Lindzon, Jared. “Why Companies Who Hire People with Disabilities Outperformed Their Peers.” Fast Company, Fast Company, 13 Mar. 2019.
News MEAction. “About.” #MillionsMissing.
“NIH Categorical Spending Report.” National Institutes of Health, U.S. Department of Health and Human Services, 24 Feb. 2020.
P. Åsbring, AL. Närvänen, et al. “Are ME/CFS Patient Organizations ‘Militant’?” Journal of Bioethical Inquiry, Springer Singapore, 3 July 2018.
Peterson, T. Mark, et al. Coverage of CFS within U.S. Medical Schools, Center for Community Research, DePaul University, Chicago, 7 Nov. 2013.
“Resources for Persons Living with HIV.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 21 Oct. 2020.
Roberts, Emmert, et al. “Mortality of People with Chronic Fatigue Syndrome: a Retrospective Cohort Study in England and Wales from the South London and Maudsley .” The Lancet, RELX, 16 Apr. 2016.
Siegel, Zachary A, et al. “A Content Analysis of Chronic Fatigue Syndrome and Myalgic Encephalomyelitis in the News from 1987 to 2013.” Chronic Illness, U.S. National Library of Medicine, Mar. 2018.
Smith, M.E. Beth, et al. “Diagnosis and Treatment of Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome July 2016 Addendum.” Diagnosis and Treatment of Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome, National Institute of Health, July 2016.
Twohig, Niall. “Beyond a Life in the Red.” The Triton, The Triton, 7 Jan. 2019.
Valdez, Ashley R, et al. “Estimating Prevalence, Demographics, and Costs of ME/CFS Using Large Scale Medical Claims Data and Machine Learning.” Frontiers in Pediatrics, Frontiers Media S.A., 8 Jan. 2019.